Convergence Blog Part One: What is EPR Convergence, and Why is it Vital to the Future of Integrated Care?
11th December 2023
In the first of a two-part blog on EPR convergence, we look at the varying definitions of the term EPR convergence for England’s health and care market and explore why the approach is fundamental to the success of integrated care.
EPR convergence is a newly developed concept for the NHS. Championed by the now-departed Tim Ferris during his tenure as National Director of NHS Transformation, the original idea was to streamline and reduce the multitude of Electronic Patient Records (EPRs) in use across acute care, community services, mental health, ambulance services, primary care, and social care.
EPR convergence aims to facilitate real-time access to comprehensive health information and seamless workflow for caregivers and to empower patients with easier access to their data.
The Perils of One-Size-Fits-All
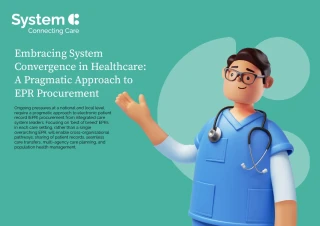
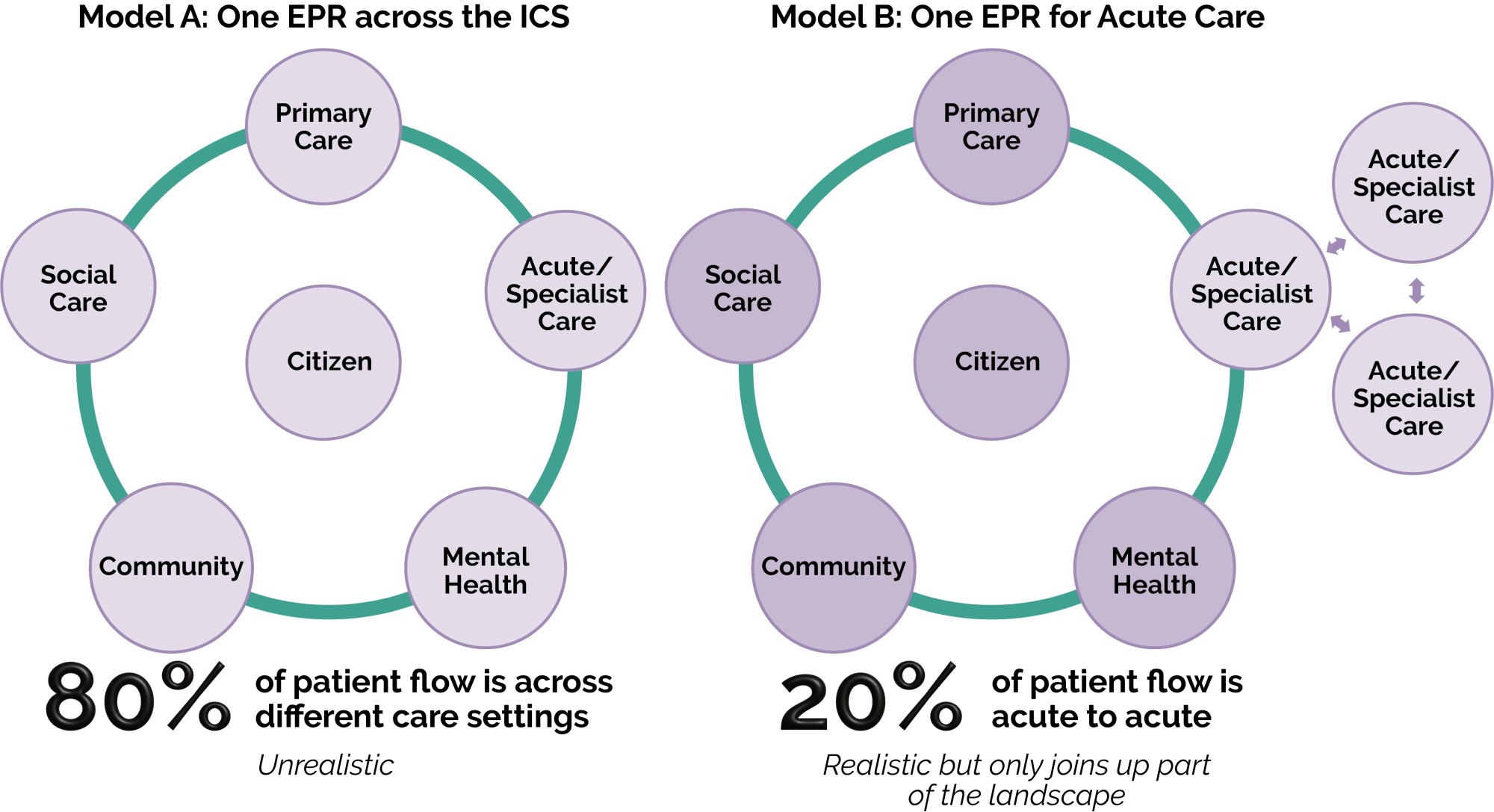
The definition of EPR convergence has changed and been interpreted differently over time. One perspective was to have ‘one EPR to rule them all’. A single system promised to provide a unified and thorough view of an individual's medical history, treatment plans, medications, and other pertinent information across care settings. This comprehensive perspective was deemed essential for delivering integrated, person-centred care – an integral aspect of current health and care policy.
With Integrated Care Systems (ICSs) leading the managed convergence of EPRs across various care settings, it has become clear that implementing the concept of a single, all-encompassing EPR is fraught with significant challenges, not least as the operational disparities among individual care settings present a huge problem.
Acute care settings, which focus on scheduling beds and clinics, operate differently from community models, which prioritise clinician time scheduling. Pathways and processes do not align across care settings.
The practicality of replacing existing systems and managing the disruption of implementing a single system across multiple settings, with no NHS precedent, further casts doubt on the viability of this approach.
While the idea of convergence seems appealing conceptually, the detailed differences in the functioning of these settings is fundamental.
Recognising these challenges, most Integrated Care Systems have shifted their focus from a one-size-fits-all EPR to a more nuanced definition of EPR convergence. Instead of pursuing a single EPR across all settings, many ICSs are choosing to converge systems within individual care settings.
Acute EPR Convergence Comes to the Fore
With this in mind, there has been particular focus on acute EPR convergence. The government set a clear target of 95% coverage by 2024 and is investing hundreds of millions to achieve this target.
Having an acute EPR is a fundamental building block for integrated care; in some cases, having all acute Trusts in an ICS makes sense, however, this approach also has its challenges. Processes must align across disparate organisations. Some organisational units may rely on systems they are reluctant to retire and may have concerns over moving to new systems, having made significant investments already.
Additionally, if convergence on to the same EPR in an ICS is the answer what is the question? With approximately 80-90% of patient flow between primary, secondary and social care, how does Acute EPR convergence help Integrated Care Systems tackle their most pressing problems like the elective backlog and expediting discharges to social care?
So, a converged EPR must go beyond the hospital's walls to enable citizen flow across the ICS or risk creating issues that could undermine the broader vision of integrated care.
Integrated Care is Evolving, and Digital Needs will do so too
The target operating model for integrated care is evolving as new structures form. A greater understanding of a population’s needs is emerging and, as a result, the digital requirements will change.
Over-investment and specification at this stage could hamper a future where a more straightforward definition of integrated care becomes a reality.
Flexibility is critical for EPRs to accommodate the diverse communication tools, shared care records, and population health platforms driving the future of integrated care and for the organisations making the investment and planning decisions around converging EPRs.
Integrated Care Partnerships can address these issues through positive collaboration, careful planning and remaining focussed on value. In our next blog, we will delve further into the approach to EPR convergence and explore how the current approach may require additional refinement to support the pursuit of more person-centred care.
Read our ebook on EPR convergence for further insight into this important topic:
Read eBook
Coming soon: watch this space for the second blog of our two-part convergence mini-series.